Understanding Hyper- and Autoinflammation
Inflammation at its worst
Canna S & Cron RQ, “Highways to Hell: Mechanism Based Management of Cytokine Storm Syndromes”, JACI 2020
Inflammation is a core pathogenic mechanism in virtually every disease process. For millenia, we’ve been focused on fighting microbes and viruses as the most important drivers of pathologic inflammation, and sepsis and its accompanying Systemic Inflammatory Response Syndrome (SIRS) remain major problems. But in the 21st century, we recognize that abnormal host responses to inflammatory stimuli can be just as deadly and destructive. In informing our understanding on host susceptibility to immunopathology, understanding how high-penetrance mutations cause inflammatory diseases has been incredibly instructive.
Autoinflammation is defined as systemic or organ-specific inflammation not attributable to infection, malignancy, or antigen-specific autoimmunity.
Hyperinflammation is a state of damaging immune activation that is excessive or disproportionate to what would be expected for a patient’s clinical context.
Our lab is interested in both, but particularly in the ways in which they intersect.
Most “autoinflammatory” patients have chronic organ-specific or systemic inflammation, but only rarely hyperinflammation. The dramatic response of many “autoinflammatory” patients to inhibition of the inflammasome-activated cytokine IL-1 has reinvigorated the quest for anti-inflammatory targets in SIRS and reinforced the therapeutic potential of targeting the inflammasome and related innate immune pathways.
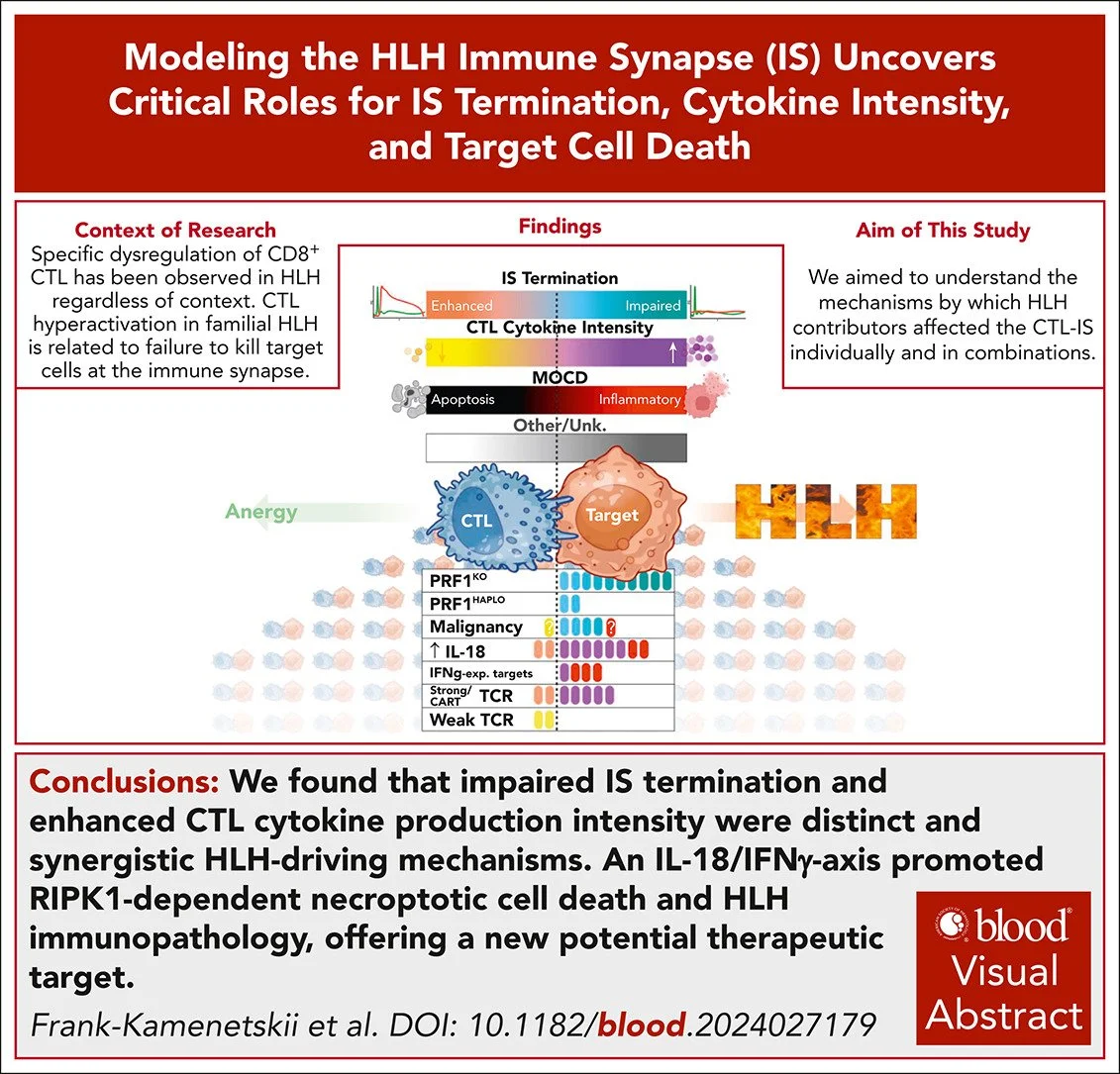
Our group studies the intersections of hyper- and auto-inflammation. In particular, we study two related disorders, Hemophagocytic Lymphohistiocytosis (HLH) and Macrophage Activation Syndrome (MAS), because they typify the concept of hyperinflammation. Whereas the pathogenesis of HLH clearly includes the inflammatory effects of defects in granule-mediated cytotoxicity, the mechanisms at work in MAS are less clear but seem to involve abnormal production and function of the inflammasome-activated cytokine IL-18. We combine clinical insights from rheumatology and innate immunity with basic models of overwhelming systemic inflammation to define new disease subtypes and disease activity biomarkers, to flesh out mechanisms of inflammatory disease, and to test promising therapeutic strategies.
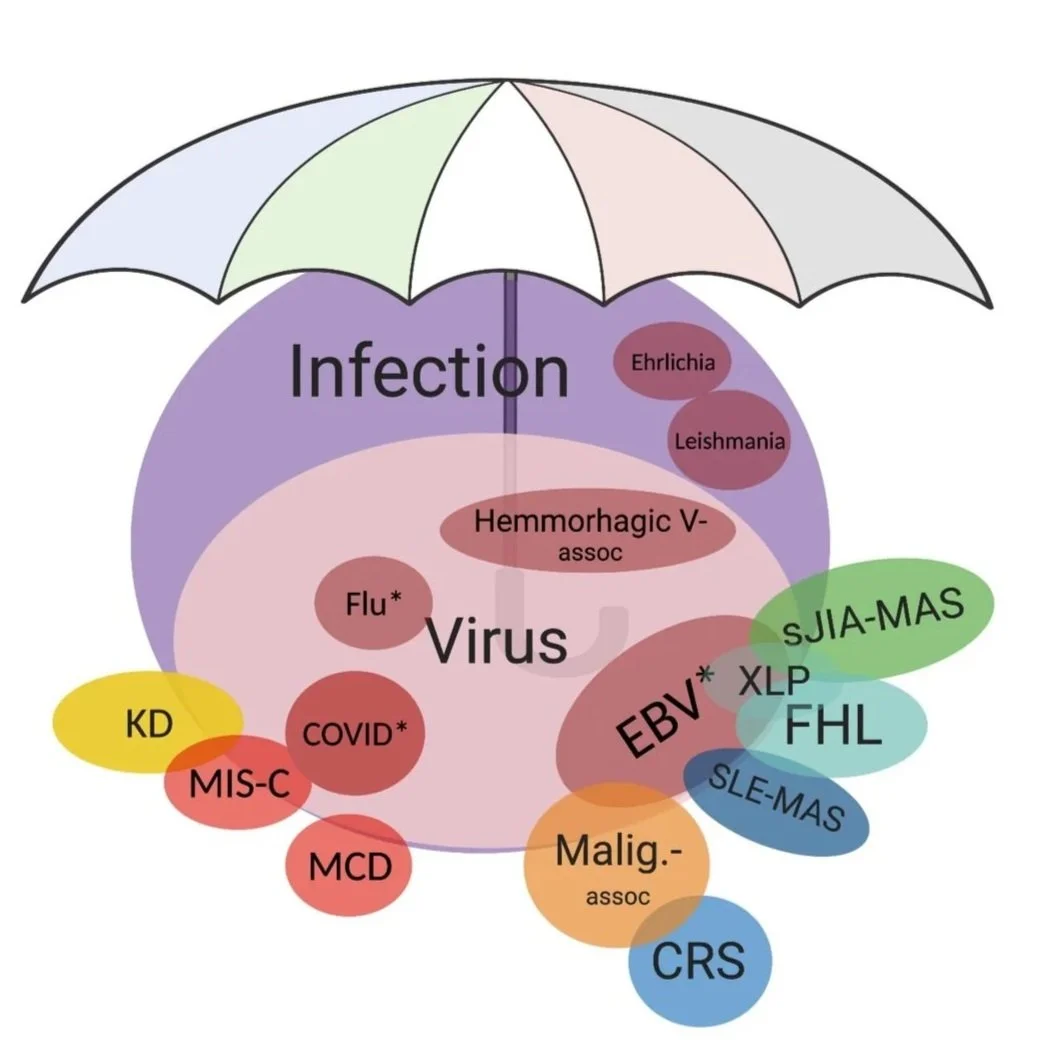
Landy et al., Nat Rev Rheum, 2024
Adapted from Henderson LA, Canna, SW, et al., Arth & Rheum, 2020. SJIA: Systemic Juvenile Idiopathic Arthritis; MAS: Macrophage Activation Syndrome; HLH: Hemophagocytic Lymphohistiocytosis; EBV: Epstein-Barr Virus; MCD: Multicentric Castelman Disease; KD: Kawasaki Disease: MIS-C: Multisystem Inflammatory Syndrome (assoc. with SARS-CoV2) in Children; ARDS: Acute Respiratory Distress Syndrome; CRS: Cytokine Release Syndrome
Goals of our Lab
I. Understand the fundamental mechanisms underlying human autoinflammatory and hyperinflammatory diseases.
II. Develop new genetic, biomarker, and functional test that better diagnose auto- and hyperinflammatory patients and monitor their disease activity.
III. Develop new therapies and therapeutic strategies that either prevent or alleviate immunopathology.
Canna S.W., and Marsh R.A., 2020, Pediatric hemophagocytic lymphohistiocytosis. Blood, vol. 135, no. 16, pp. 1332-1343.
On Diversity, Equity, and Inclusion
We recognize that our lab arose within and exists to serve an evolving society and community. We strive to recognize and improve upon the faults and failures of that society. As such, our lab is a safe space to be yourself, speak up, be creative, and make mistakes. However, we expect members to be productive, reliable, conscientious, and ambitious. We are charged with pushing the boundaries of scientific understanding and making discoveries that change patients’ lives. DEI matters to us because good science requires a space where all voices and opinions can contribute. In this work, we can be a vehicle for social improvement by working to ensure:
we provide opportunities and rigorous training to a diverse workforce
we address problems that affect all patients
we work with health systems, insurers, and patient organizations to make sure our efforts and discoveries benefit all.
But words on a webpage don’t amount to much, the real work happens in the lab.